The United States and United Kingdom both shifted their policy paths around a similar time. The two countries which had maintained a somewhat lukewarm attitude, adopted strong social distancing measures starting from mid-March. Behind this policy shift is an Imperial College London report written by the school’s COVID-19 Response Team titled “Impact of Non-pharmaceutical Interventions to Reduce COVID-19 Mortality and Healthcare Demand.”
Simulating the spread of COVID-19 through its model, the report estimated 510,000 total deaths in the UK and a staggering 2.2 million deaths in the US if there are no interventions by the government. The Response Team apparently gave this report to Washington and London before its official release on March 16 according the Guardian in its article “New Data, New Policy: Why UK’s Coronavirus Strategy Changed.” CNN followed this up by reporting that the “US, UK coronavirus strategies shifted following UK epidemiologists’ ominous report.”
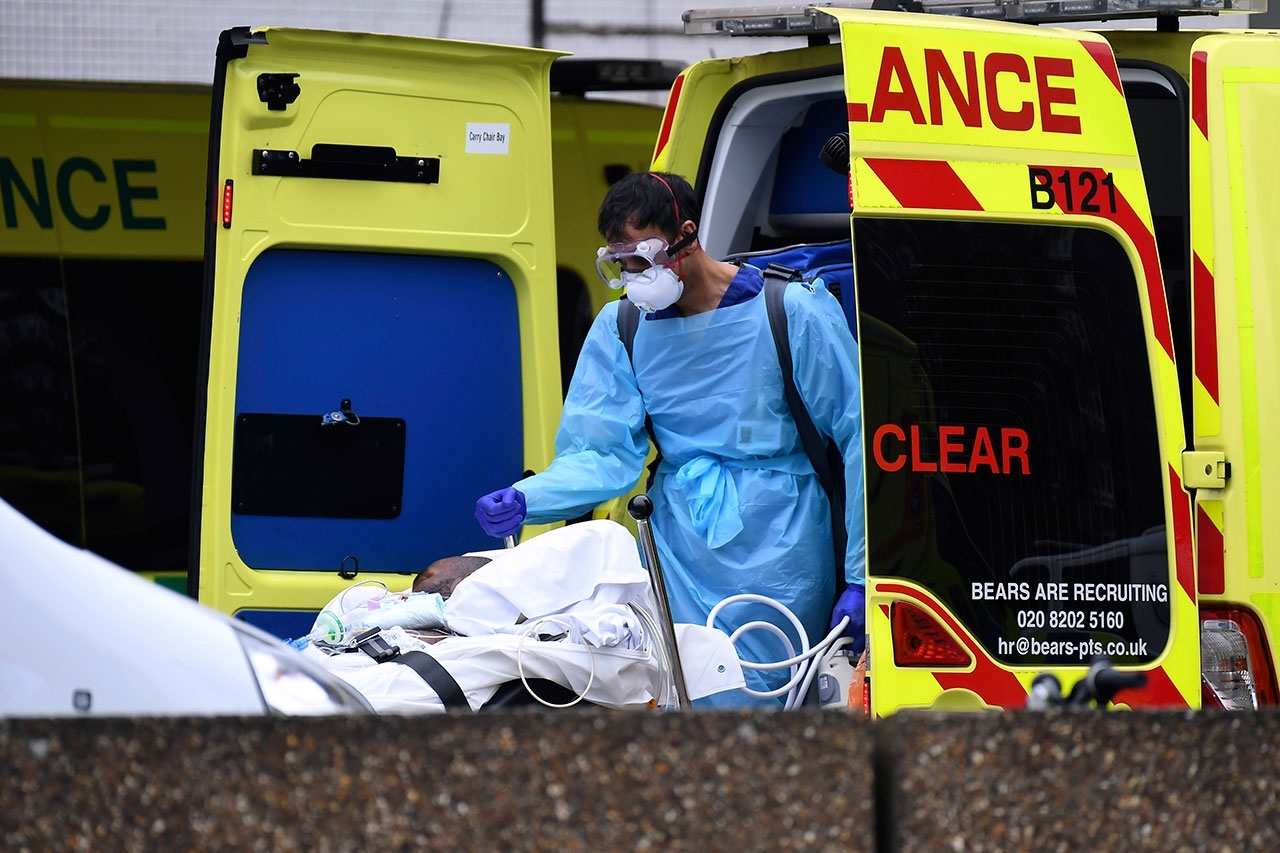
This report reviewed a few scenarios that would prevent the worst possible cases. According to the report, a ‘mitigation’ strategy, which would comprise the least intervention, cannot stop ICU beds from flooding with coronavirus patients. Only a ‘suppression’ strategy—which would include quarantine, school closings and social distancing—would prevent a total collapse of the healthcare system owing to overflowing coronavirus patients (See Graph #1). President Trump who had brushed off the novel coronavirus as nothing more serious than a seasonal flu,announced a new set of stronger social distancing guidelines on March 16, advising Americans to work from home and stop dining out. The British government also strengthened measures on the same day, steering away from the previous herd immunity strategy. From March, the number of total cases started to escalate rapidly along with the death count. If there hadn’t been the Imperial College report, the two countries would have faced an even harsher reality.
Different COVID-19 simulation reports are gushing out as the pandemic prolongs. Some of them are based on concrete scientific research, but others are nothing more than an oracle. It would be wishful thinking to assume simulations like calculators can provide answers by punching in a few numbers; but they can become a key tool to look at ways to solve this difficult problem of facing an unprecedented pandemic. SisaIN looked into a simulation model drawn out by a South Korean research team.

Simulations in February: How to Avoid the Worst
The Korean National Institution for Mathematical Science (KNIMS) has a Research Team that is one of a few expert groups dedicated to building a COVID-19 simulation model. Scientists from a wide range of fields are part of this team, and many of them also cover several areas of expertise. The leader of the Imperial College Response Team, Neal Ferguson, is often introduced as both epidemiologist and mathematical biologist, for instance. Similarly, Woo-Sik Son of the KNIMS Research Team has a Ph.D. in physics, and the rest of his team have degrees in mathematics and physics. KNIMS Research Team is a part of a Government-wide R&D Fund Project for Infectious Disease Research (GFID), a cross-ministry organization inside the South Korean government created after the 2009 swine flu and 2015 MERS outbreaks to facilitate government response against a pandemic. Specialists of preventive medicine, infectious diseases and medical data all joined GFID, providing essential feedback to help the KNIMS Research Team develop a more precise coronavirus simulation model.
The most often-used infectious disease simulation model is the compartment model. It classifies the population into different groups according to their infection status. The most simple way for this classification is the SIR Model which labels the population into three groups: Susceptible(S), Infectious(I), and Recovered(R). Those who are susceptible become infectious depending on the rate of infection.
The number of population “compartments” differ depending on the circumstances of a given society and the characteristics of the infectious disease. The KNIMS Research Team created a 2019-nCOV domestic infection spread model in early February, when the total COVID-19 cases in South Korea remained below 30. The team used the SEIR Model instead of SIR, adding the Exposed(E) classification between those who are Susceptible and Infectious. Those who in the exposed category are infected but are not infectious yet due to low virus count (See Graph #2). The Research team also divided the entire population of South Korea into 250 regional provinces and reflected various population movement patterns across the different provinces and within each region. Without taking both short and long-distance travel patterns into account, the model would calculate that a patient in Daejeon would be equally likely to infect his/her close-by neighbors and a random stranger 150 kilometers away in Seoul. This would greatly diminish the accuracy of the simulation.
There wasn’t much domestic data on COVID-19 up until February. The KNIMS Research Team referenced the datasets from Wuhan, which had been collected by a team of Hong Kong researchers. The estimated average basic reproduction number (R0), the expected number of cases directly generated by one infectious patient, was set as 2.68. The Research Team designed the simulation model based on a hypothetical scenario where a coronavirus patient diagnosed in Jongno District, Seoul starts local transmission from January 28. The results were grave. The daily number of new cases would exceed 900,000 by June 1.
“It was totally crazy; all the results were similar,” recalled Son. “Most of the simulation reports published in the medical journal like The Lancet showed similar terrifying results.”
Based on this simulation result, the Research Team estimated the efficacy of various preventive measures. From left to right, the graphs on Chart #3 show how the estimated number of coronavirus patients changes as stricter rules are enforced on long-distance travel. An efficient set of preventive measures would reduce the count of the patient’s peak-time or delay the arrival of the peak; but the graphs did not differ much irrespective of the degree of enforcement on long-distance travel. On the other hand, preventive measures centered around social distancing and personal hygiene such as washing hands and wearing masks were very effective. On Chart #3, as moving down on different graphs, one can see different simulation results from stronger social distancing and personal hygiene: the peak arrives later, and confirmed cases reduce dramatically. This is the way the South Korean government is successfully limiting the spread of COVID-19, by adopting stronger social distancing measures rather than restricting long-distance travels.

Simulations in March: What Happened in Daegu?
The large-scale mass infection in Daegu after the appearance on February 18 of patient 31, a follower of the Shicheonji Church, was a rare probability event beyond the range covered by the simulation model.
“The church conducted masses in very close contact and was unwilling to share information for their secretive nature,” said Son. “That’s why they became a high risk group. This is an extremely uncommon event, statistically far skewed to one extreme end.”
The KNIMS Reaserch Team started developing in early March another simulation model to estimate the spread of coronavirus in Daegu. The researchers could not use the same model initially created for a nationwide prediction. In order to correctly simulate under the regional circumstances of Daegu, the model needed to reflect a special population compartment: the Shincheonji Church of Jesus. It also had to include other communities such as families, schools and workplaces, which could be separate compartments in tracing contacts and, therefore, the virus itself. The families with Shincheonji churchgoers and those without would have different chances of spreading the virus, for example.


The Research Team adopted a microsimulation model. This model assumed a virtual community with the population size of Daegu and simulated the spread of an infectious disease. Using the population census from 2015, the model created a population composition similar to that of Daegu and randomly selected 9,000 Shincheonji followers out of 2.5 million Daegu citizens. The team also added a Hospitalization(H) compartment in addition to the SEIR (Susceptible, Exposed, Infectious and Recovered) compartments to reflect quarantine and isolation that follow after diagnosis or possible exposure to the virus (See Graph #2). The COVID-19 spread was reenacted as Graph #4 illustrates. It shows how the infections among the Shincheonji churchgoers spread all across the Daegu citizens through families, schools and workplaces.
Through this simulation process, the Research Team found a separate infection probability for Shincheonji followers and other Daegu citizens. According to this model, the chances of infection among Shincheonji followers was 3.06, while it was 0.31 among other Daegu citizens. Shincheonji churchgoers were 9.3 times more likely to get infected by the coronavirus. Owing to quarantine measures adopted by the government such as church shutdown and isolation, the coronavirus infection probability among Shincheonji members has been zero since February 29. The Research Team predicted that the COVID-19 spread in Daegu from March would depend on the infection probability among non-Shincheonji citizens and that the last coronavirus patient in Daegu would be diagnosed around April 26. The coronavirus spread would have been overestimated if the simulation had been done without distinguishing Shincheonji believers and regular Daegu citizens.
After April: When Will All This End?
It has become common knowledge that a pandemic ends when the basic reproduction number (R0) becomes smaller than one: If R0 equals 0.5, it means the total patient count has halved over time and eventually converge to zero. To be exact, what changes over time is not R0 but Rt: the time-dependent reproduction rate, an important parameter that measures the secondary number of cases caused by each infected patient. It is calculated by multiplying pathogen infectivity, contact frequency with the infected patients, and duration of infection spread.
Pathogen infectivity is a constant, which depends on biochemical characteristics of the coronavirus itself, but the other two components differ depending on how a community responds to the pandemic. Social distancing reduces contact frequency with the infected patients, while contact tracing, quarantine and isolation cap how long the virus will spread.
“It seems like the Rt value in Seoul has dropped below zero,” said Son.
The Rt value in South Korea is estimated at 0.679 as of April 15, according to Seoul Asan Medical Center’s Medical Imaging & Intelligent Reality Laboratory. Other research teams overseas also estimate South Korea’s Rt value to be less than 1. A research team in Peking University estimated the Rt value at 0.3 and predicted that the coronavirus pandemic in South Korea will end sometime between September 4 and 24.
However, the end of the pandemic does not mean that South Koreans can go back to the life they had before it all started. Revisiting the Imperial College report on Graph #1, the green and orange graphs, which indicate the number of critical patients, stay below the maximum ICU bed capacity reflected by the red graph while suppression measures are still in place. When suppression is over, however, the green and orange graphs that had been suppressed spike. Unless a vaccine is developed soon, when intervention like social distancing is not enforced, COVID-19 patients will begin to increase soon again.
“That [Imperial College] report is not a particular, pessimistic report,” said Son. “All simulations show similar tendencies. Unless there is a vaccine, and most of the people become immune, we cannot loosen up.”
Another GFID cooperative organization, the Korean National Cancer Center, reports that COVID-19 cases will skyrocket if strict social distancing measures are lifted. According to the KNCC report, if the domestic contact level that has been reduced by 75%, climbs back up to half of the usual times, the total number of coronavirus cases will increase to 43,569 by May 9.
Facing a pandemic is painful but nothing about it will not bring answers or create solutions. Infectious disease simulation models can be a lamplight that lights up the way ahead while navigating through an unprecedented COVID-19 pandemic.
“It is actually a dangerous task, since you have to make a prediction with an exact number,” said Son. “When things are advancing in real-time, a simulation model sometimes expires within a week. We still have to make predictions regardless, just like we still continue forecasting the weather although it is often incorrect.”
Why the government insists on “quarantine measures in daily life.”
How are infectious disease simulations being used in real life? What is the best way to understand these simulation results? SisaIN asked Kim Jong-Hun, a preventive medicine doctor at Sungkyunkwan University working for the Gyeonggi Infectious Disease Control Center, one of South Korea’s local COVID-19 prevention teams.

Since when simulation models were being used to stop the spread of infectious diseases?
Mathematical modelings go back to the 1920s. It is in fact a very simple model, and the core of the SEIR (Susceptible, Exposed, Infectious, Recovered) model has not changed much. When a pandemic hits, we cannot prepare for it unless we predict the size of an incoming spread. We need to know some precise set of data on how many ICU beds are needed or how many ventilators should be prepared.
Simulations tell us that when we loosen up social distancing, confirmed cases will increase again.
Citizens often misunderstand that quarantine measures such as social distancing can get rid of the virus. They are simply preventive ways to evade it. A pandemic ends when we acquire herd immunity through vaccines or when the majority of the population recover from the virus after having been infected. That is the context behind the news headlines that “the world cannot return to the world before COVID-19” or that the government is preparing for a continued set of quarantine measures. This will continue to be a marathon until a vaccine is developed.
Will all the quarantine efforts be meaningless if there is no vaccine?
That’s not true. It is important to suppress the curve so that the healthcare system can handle all patients. That’s the only way to stop the death of patients who were not able to receive any medical attention. It is not just the virus that that kills people. We need to maintain medical capacity for other patients suffering from other illnesses also. We must be able to manage and prepare a better medical system.
Is there significant value in reading COVID-19 simulations?
Rt value is a good reference point. If Rt value continues to rise, then it means quarantine measures are not working: Rt value should stay under one. If a mass infection is occurring, then experts on the ground should notice. Sporadic infections, on the other hand, are not easy to detect .
Sometimes simulation results are not accurate enough for policymakers to use as a reference point in building practical quarantine measures.
Some predictions seem like they are just rolling it for fun (laughs). For professional expert teams specializing in infectious disease simulation, there are fundamental obstacles that are hard to overcome. The final results vary significantly on whether a single patient can infect 2.5 or three patients. Since things are moving in real-time, those parameters are in constant change.
How should the general public understand and utilize the simulation results?
The direction to which the results are pointing matter more than the numbers. It is a better approach to look at the progression of the numbers, like “if this trend continues, then this is how things will go. If relaxed social distancing measures are adopted, new daily confirmed cases will implode by a couple dozen times.”
translated by Minho Kim
translation supervised by Beckhee Cho


